10Bertha Roentgen’s Wedding Ring
In November 1895, physics professor Wilhelm Conrad Roentgen of Worzburg, Bavaria, was studying electrical rays when he discovered that they penetrated objects and projected their images on a fluorescent screen. When he put his own hand in front of the rays, he noticed that the image showed a contrast between his bones and his translucent flesh. Roentgen realized the implications immediately—doctors could see a person’s anatomy and anything wrong with it without evasively opening the skin. He replaced the fluorescent screen with a photographic plate and captured the first X-ray image on November 8, 1895. The X-ray was of his wife Bertha’s left hand and her wedding ring (as pictured above). The world was initially dubious about Roentgen’s discovery. The New York Times spurned it as a simple photographic technique that had already been discovered. Just a week later, however, the Times began to run reports about how Roentgen’s X-rays were in fact beneficial for surgical purposes. One of those reports were of a British doctor named John Hall-Edwards who was the first to use X-rays to diagnose a problem—a needle lodged in a hand. Roentgen received the 1901 Nobel Prize in physics, and his findings are now considered “one of the greatest discoveries in the history of science.”
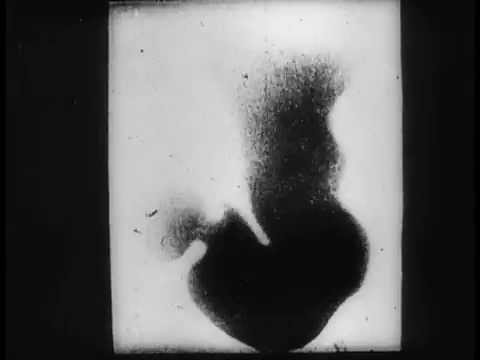
9Moving X-Rays Of The Heart And Digestive System
Things moved quickly after Roentgen’s discovery. Almost immediately, scientists worked to merge X-rays with cinematography—essentially moving X-rays. The first to produce one was John Macintyre, a throat surgeon and electrician at the Glasgow Royal Infirmary. Macintyre already had the distinction of setting up the world’s first X-ray department, and his unit would later be the first to X-ray a foreign object (a halfpenny lodged in a child’s throat). That unit also was the first to detect a kidney stone with an X-ray. In 1897, Macintyre presented a short film at the London Royal Society demonstrating what he called a cinematograph. He had X-rayed a frog’s leg since it required less energy to penetrate than a human leg. He then X-rayed it every 300th of a second as he flexed and extended the leg. He then spliced them together. Later, he filmed a human’s beating heart. He also fed a patient bismuth and filmed his stomach as he digested it (see video above). These X-ray movies are now called “fluoroscopy” and are used to film the placement of heart catheters, the digestive and urinary systems at work, and surgical procedures. In 2013, 1.3 million fluoroscopic procedures were performed in the United Kingdom alone.
8Major Beevor Hunts For Bullets
Within months of Roentgen’s discovery, X-rays were used on the battlefield. They were first used during the Abyssinian War when Italy invaded Abyssinia in 1896. Lieutenant Colonel Giuseppe Alvaro used an X-ray machine to locate bullets in the forearms of Italian soldiers. Those X-rays have since been lost to history. A year later, X-rays were again used in the field during the Greco-Turkish War. Those films have also been lost. Despite multiple successes, the military was slow to appreciate the use of X-ray for their wounded. In June 1897, war broke out between India and Afghanistan. Britain sent soldiers to the Tirah plateau to open the mountain passes. Major Walter Beevor purchased X-ray equipment and set it up at a field hospital at Tirah. He took more than 200 X-rays in the field including the one above of an Indian soldier’s elbow with a bullet lodged in it. Beevor even located a bullet lodged in General Woodhouse’s leg. The next year Beevor made a presentation at the United Services Institution—from then on, Britain brought field X-ray units onto the battlefield. Other countries slowly followed suit. Like many other technologies, X-ray imaging benefited from its use in war. One of those advances was in portable units. Marie Curie and her daughter Irene drove 20 X-ray units in the back of vans to the battlefront during World War I. Today, mobile X-ray machines are brought to a patient’s bedside, taking radiographs of them when they are too sick to be moved to the hospital’s radiology department.
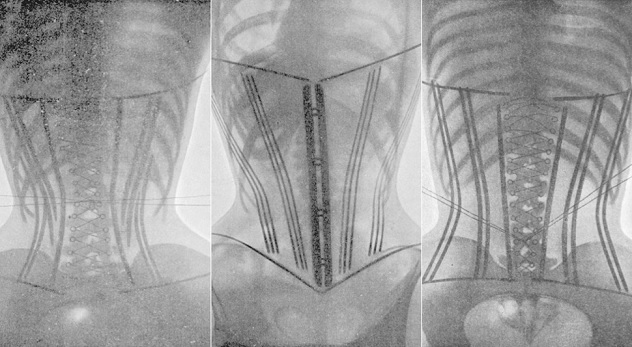
7Proof Of The Damage Caused By Metal Corsets
In one of the earliest known uses of medical imaging to raise public awareness of a problem, French doctor Ludovic O’Followell X-rayed the torsos of several women with and without corsets. The films clearly show that tight metal corsets narrowed the ribcage and displaced internal organs. O’Followell did not advocate the banning of corsets—merely the development of more flexible ones. And that’s exactly what happened. O’Followell’s films, along with the opinions of other physicians of the time, influenced the industry and society to adopt less-restrictive corsets. The question that later experts asked was whether O’Followell should have used X-ray radiation to prove his point. Back then, X-ray units required the subject to be exposed to radiation for lengthy periods of time. In 1896, an X-ray of a man’s forearm required 45 minutes of exposure. The first dental X-ray took 25 minutes. The women in the X-rays above were exposed twice—both with and without a corset—and in the most radiation-sensitive parts of their body: the chest (breasts and sternum) and the abdomen (reproductive organs). The dangers of X-ray radiation exposure was already well-known. In the first year of testing X-rays, a Nebraska doctor reported cases of hair loss, reddening and sloughing off of skin, and lesions. Clarence Dally, while working on X-rays for Thomas Edison, repeatedly exposed his hands to radiation for at least two years. He had both arms amputated before dying of cancer in 1904. One by one, the pioneers of the field—John Hall-Edwards, Marie and Irene Curie, and Wilhelm Roentgen—all died of radiation-induced diseases. But the world was slow to realize the dangers of unnecessary X-rays. Women had their ovaries irradiated as a treatment for depression. Radiation was used to treat ringworm, acne, impotence, arthritis, ulcers, and even cancer. Beauty shops irradiated customers to remove facial hair. Water, chocolate, and toothpaste were spiked with radiation. Between the 1920s and the 1950s, many shoe stores had fluoroscopes—called Foot-o-scopes or Pedoscopes—that X-rayed customers’ feet to show how well their shoes fit. While X-rays are much safer today and are almost never used for non-medical purposes, unnecessary medical X-rays still pose some risk. One study showed that 18,500 cases of cancer worldwide are the result of medical X-rays, and in America 0.5 percent of cancer deaths are attributable to X-rays.
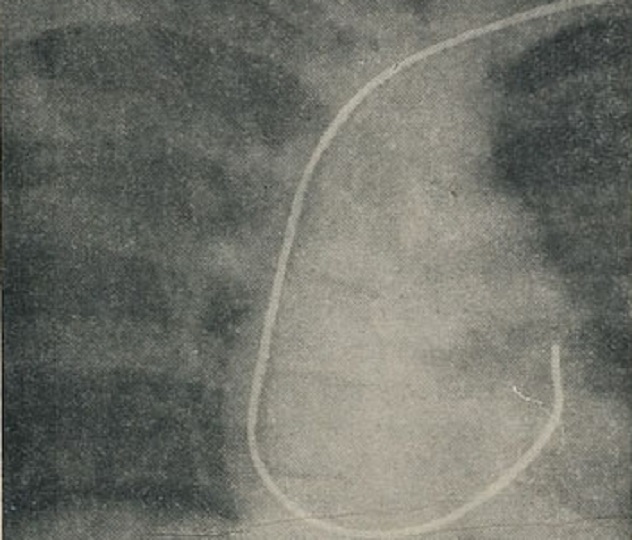
6The Very First Catheter
While working as a surgeon at the August Victory clinic, Werner Forssmann developed a theory that a flexible tube (catheter) could be inserted in the groin or arm, through the veins that feed blood to the heart, and directly into the heart’s atrium. Forssmann believed that the heart’s volume and the blood’s flow rate, pressure, and oxygen content could be measured with this catheter. Medicine could also be directly injected to the heart in an emergency. Most experts believed the catheter would get tangled among the surge of blood and the beat of the heart. Therefore, his superiors at August Victory would not sanction experiments conducted by the rookie doctor. Undeterred, Forssmann convinced a fellow resident to insert a needle into his left arm. Then, Forssmann advanced the catheter up the resident’s cephalic vein, through the bicep, past the shoulder, and into the heart. It took a total of 60 centimeters (2 ft) of tubing. He then walked down to the X-ray department and took a picture to prove the catheter was in the resident’s heart. He later performed the procedure several times on himself. Unfortunately, Forssmann’s colleagues derided this procedure as a mere circus stunt. Discouraged, Forssmann moved on, becoming an urologist. He was unaware that his contribution was gradually being recognized for its importance (by 2006, 3.7 million heart catheterizations were performed annually in the United States alone). So he was quite puzzled when he received a phone call in October 1956, informing him that he’d won the Noble Prize in Physiology and Medicine. He simply responded, “For what?”
5Hyperphonography
One of the drawbacks of X-ray technology is that it only images dense anatomical structures such as bones and foreign bodies (like bullets). Another drawback is that it uses radiation that could harm a baby in the womb. The medical world needed a safer way to image less-dense structures in the body. The answer came from a tragedy: the sinking of the Titanic in 1912. In order to better detect icebergs, Reginald Fessenden patented devices that emitted directed sound waves and measured their reflection in order to detect distant objects. His sonar was capable of detecting icebergs from a couple miles away. World War I erupted at the same time, and German U-boats threatened Allied shipping. Physicist Paul Langevin developed a hydrophone that used sound waves to detect submarines. On April 23, 1916, a UC-3 U-boat became the first submarine detected by hydrophone and sunk. After the war, the technology was used to detect flaws in metals. In the late 1930s, German psychiatrist and neurologist Dr. Karl Dussik believed that sound could measure the brain and other parts of the body inaccessible by X-rays. Dussik became the first to apply sound diagnostically. Unfortunately, much of his work was performed in Austria—it wasn’t until after the war, when he repeated and expanded his work, that the world heard of what he called “hyperphonography.” A decade later, Scotland obstetrician Ian Donald borrowed an industrial ultrasound machine and tested it on various tumors. Donald was soon using the machine to detect tumors and monitor fetuses.
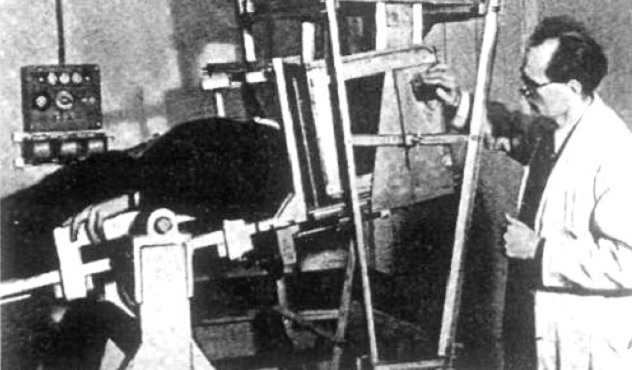
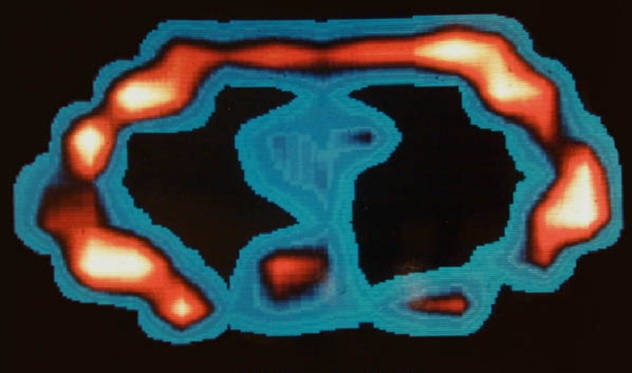
4The First CAT Scan
One limitation of X-ray images is that everything between the X-ray tube and the film appears on the image. Pathologies such as tumors can be hidden by tissues, organs, and bones that lie above or below it. The 1920s and ’30s saw the development of tomography. This took an X-ray at a certain level of the body, blurring anything above and below it. It did this by moving the X-ray tube (and film) while exposing the image. It could cut across all three planes of the body: sagittal (left to right sides), coronal (front to back), and axial or cross-sectional (feet to head). In 1967, Godfrey Hounsfield, a scientist working for EMI (Electric and Musical Industries), thought up an axial tomographic scanner. EMI was also the record company that sold 200 million Beatles records. Using their Fab Four funds, EMI funded Hounsfield for the four years it took for him to develop a prototype. His scanner used sensors instead of film, and the patient was slid through moving tubes and sensors at a proscribed pace. A computer then reconstructed the anatomy. Hounsfield’s invention was thus dubbed a computed axial tomographic scan or CAT scan (now simply CT scan). On October 1, 1971, Hounsfield used his invention for the first time. He located a woman’s brain tumor as seen here. The oval on the left side of the film (her right frontal lobe) is the tumor. Later, after the surgeon removed the tumor, he remarked that it “look[ed] exactly like the picture.”
3The First MRI Scan
In a Magnetic Resonance Imaging (MRI) scan, the machine creates a static magnetic field that aligns all of the patient’s protons in the same direction. Short bursts of radio waves then misalign the protons and, once the radio waves are shut off, a computer measures the time it takes for the protons to realign. The computer then uses these measurements to reconstruct the image of the patient’s body. While CT and MRI machines look similar, they are very different. CT scans use potentially hazardous radiation while MRI does not. An MRI can also visualize soft tissue, organs, and bones better than CT. It is used especially when the doctor wants to see the spinal cord, tendons, and ligaments. On the other hand, CT is better to see bone, organ, and spine damage. Physician Raymond Damadian first conceived of a whole-body MRI scanner in 1969. He began testing his theories and published an article in Science Magazine in March 1971. In September of that year, Paul Lauterbur, a chemist at State University of New York, had an epiphany about the very same thing, and even bought a notebook to document his “invention.” Lauterbur later admitted that he had watched a graduate student reproduce Damadian’s experiment, but did not believe it would work. In March 1972, Damadian filed a patent for his idea. That same month, Lauterbur’s scanner produced an image of test tubes. A year later, Lauterbur published his findings and his image in Nature. He did not refer to Damadian’s critical contributions. In 1974, Damadian’s patent was accepted. Then on July 3, 1977, Damadian and his team took the first scan of a human. None of his staff wanted to climb into the machine, so Damadian did it himself. When it didn’t work, they speculated that the doctor was too big. One of his graduate students, Larry Minkoff, was thinner and climbed in. The above image is of Minkoff’s chest. A fight then erupted between Lauterbur and Damadian over who invented the MRI. Despite the fact that Damadian held the patent, was inducted into the National Inventors Hall of Fame in 1988, and was acknowledged as the inventor by President Ronald Reagan, the 2003 Nobel Prize went to Lauterbur. Despite the Nobel committee being able to name up to three recipients of the prize, Damadian was snubbed. His supporters claim he was ignored because he was an outspoken Christian and advocate of creationism which was frowned upon by academia.
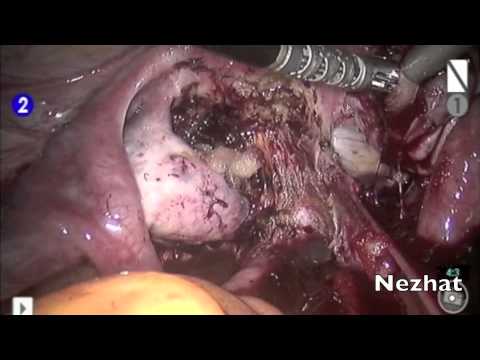
2Laparoscopic Surgery
Surgeons have been removing things from people’s abdomens for centuries, but the entire abdomen always had to be opened. This made the patient susceptible to infections and required long recovery times. But in 1901, a Russian gynecologist introduced laparoscopy—surgery done not through a large opening but through one or more small slits or holes. This came to be called “key-hole” or “Band-Aid” surgery. Laparoscopes allowed the surgeon to use one eye to look directly into the abdomen or chest with a device that resembled a small telescope. Instead of using their hands, they utilized scissors, forceps, clamps, and other tools on long rods that were inserted through adjoining holes in the abdomen. Unfortunately, this meant that the surgeon had to contort his body in order to view the laparoscope. One surgeon remembered he had to lie on the patient’s thigh in order to remove her gallbladder. After 2.5 hours, he was physically exhausted. For that reason, laparoscopy saw only limited use. In the late 1970s, Dr. Camran Nezhat, an obstetrician and gynecologist, attached video equipment to laparoscopes and operated watching a television monitor. The equipment was initially big and bulky, but Nezhat embraced technology that streamlined equipment and magnified the images. This allowed everyone in the operating room to watch what the surgeon was doing. As Nezhat put it, surgery went from a “one-man band” to an “orchestra.” Nezhat’s early videos are not available, but the above video is of a laparscopic removal of a gallbladder by another surgeon. Nezhat believed that most surgical procedures could be done laparoscopically rather than with huge evasive holes in the patient’s body. Many others could not believe that complicated surgeries could be done this way and were hostile to Nezhat’s claims. His procedures were called “bizarre” and “barbaric.” When others embraced laparoscopy, they too were ridiculed. But by 2004, when the New England Journal of Medicine recommended laparoscopy, Nezhat had officially ushered in a revolution in surgery.
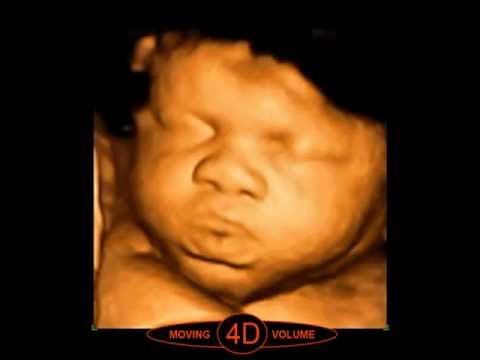
13-D And 4-D Ultrasounds
For 30 years, ultrasounds were limited to two dimensions, where equipment would send a sound and then measure the echo. Millions of parents have tried and failed to glean from these black-and-white images just what their baby looks like. This is because 2-D scans go right through the baby’s skin, visualizing their internal organs instead. Since the 1970s, investigators had been working on 3-D ultrasound for babies. This sends the sounds in different directions and angles, catches the facial features and skin of the baby, then reconstructs the echoes in much the same way CT scanners do. In 1984, Kazunori Baba at Tokyo’s Institute of Medical Electronics was the first to obtain 3-D images of a baby in the womb. But the quality of the image and the amount of time that it took to reconstruct the image (10 minutes) made it unsuitable diagnostically. In 1987, Olaf Von Ramm and Stephen Smith patented the first high-speed 3-D ultrasound that increased the quality and reduced the processing time. Since then, there has been an explosion in ultrasounds, especially with the addition of 4-D versions where the parents can see their baby move. Boutiques have even sprung up that offer 3-D and 4-D video keepsakes—for a hefty price tag naturally. While there are no documented negative effects from these ultrasounds, a debate now rages over whether a diagnostic tool should be used in such a recreational way. Steve is the author of 366 Days in Abraham Lincoln’s Presidency: the Private, Political, and Military Decisions of America’s Greatest President.