Society has moved from tepidly prodding psychology with a long stick to an almost cult-like fascination and macabre fetishization of the concept. Comic books, TV shows, and movies almost always generate a buzz with the strategic use of the word “crazy.” Were that not the case, how much differently would Heath Ledger’s Joker performance have been received? Buzzwords like “psychopath,” “insane,” and “sociopath” are top contenders for words that are most frequently used despite a general misunderstanding of their meanings, right up there with “ironic” and “rhetorical.” Schizophrenia is another one of those hot buzzwords that gets passed around corners in hushed tones but is rarely (accurately) expounded upon. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) defines schizophrenia as the presence of “two or more of the following symptoms for a significant portion of time during a 1-month period (or less if successfully treated): (1) delusions (2) hallucinations (3) disorganized speech (e.g., frequent derailment or incoherence (4) grossly disorganized or catatonic behaviour (5) negative symptoms, i.e., affective flattening, alogia (poverty of speech), or avolition (lack of motivation).” (Note: The DSM-V terminology is essentially the same.) The psychological community has examined schizophrenia with an increasingly stronger lens since the beginning of the 21st century, and they have made many surprising findings.
10 Schizophrenia Is The Result Of Over-Intense Mental Processing
A common misconception about schizophrenia is that those who suffer from it have weaker mental processing skills, which many believe is to blame for paranoid delusions and inaccurate memories. On the contrary, neural activity tests have provided evidence supporting the exact opposite explanation. If you’ve ever been guilty of throwing back a shot or five too many on Cinco de Mayo, then you might be familiar with the phrase, “Follow my finger.” The follow-my-finger sobriety test is an example of more than just why you should usually have more water in your body than tequila; it’s an example of what psychology wizards refer to as saccadic eye movement. To put it simply, your brain processes resources and memories differently when your eyes are in motion, as opposed to a static point of view. Scientists at the UC Davis Center for Mind and Brain conducted a test that focused on saccadic eye movement. The purpose of the study was to distinguish between the eye-movement (EM) brain activity of people with schizophrenia and healthy control subjects without the disease. All of the participants were asked to shift their eyes to a “target” in their peripheral vision, while avoiding a “non-target” closer to the center of vision—the catch was that they all had to keep a certain random color in mind during the exercise. The hypothesis was that the non-target would be more distracting to the participant if its color matched the one that they were asked to keep in mind during the exercise. The results showed that the effect of matching color between the non-target and the imagined color was much more intense in participants with schizophrenia than those without. It was also observed that participants with schizophrenia were prone to hyper-focus on the space surrounding the main target’s position. The findings served as more support to the belief that schizophrenic symptoms might actually be the result of a super-narrow, abnormally intense level of resource processing than normal.
9 Schizophrenia Is Linked With Brain Areas That Process Cannabis
Whenever somebody suggests that cannabis “kills the brain,” chances are that they’ve never heard of something called the endocannabinoid system (ECB). The ECB is a part of brain that modern science has found to be specially fine-tuned to reception of cannabinoids for emotional processing, memory maintenance, and learning. The existence of the ECB is not evidence that lighting up in your parents’ basement actually makes you a genius, but its discovery helped us understand the brain a lot better and also raised many more questions. The existence of cannabinoid receptors provoked questions such as “why do we have cannabinoid receptors in the first place?” and “how do cannabinoid receptors interact with mental diseases?” Scientists at the Department of Anatomy and Cell Biology at the University of Western Ontario conducted a study to address the latter question, specifically focusing on schizophrenia. The heavily cited report states that the medial prefrontal cortex (PFC) and the basolateral nucleus of the amyglyda (BLA) are not only both cannabinoid receptor–heavy areas that are extremely important for emotional regulation but are also prone to serious distortions in cases of schizophrenia. In addition to the relationship between cannabinoids and schizophrenia-affective brain regions, research conducted at the University of Western Ontario’s labs also reported a strong interaction between cannabinoid transmission and dopamine. Dopamine is a neurotransmitter that’s been found to be essential in explaining addiction and schizophrenic pathology.
8 Schizophrenics’ Memories Are More Resilient To Long-Term Substance Abuse
Up until very recently, there hasn’t been much research done on the effects of long-term substance abuse on the working memories of people with schizophrenia. The relationship between schizophrenia and poorer memory is well documented, as is the relationship between substance abuse and forgetting your entire weekend. Less well-studied is the impairment of base-level memory by substance abuse of schizophrenics. Drs. Jessica A. Wojtalik and Deanna Barch of the Washington University School of Medicine conducted a study to provide some much-needed data in this area. Thirty-seven schizophrenia patients (17 with a history of substance abuse and 20 non–substance abusers) and 32 non-schizophrenic controls (12 with a history of substance abuse and 20 non–substance abusers) completed a working memory task while being scanned with an fMRI. The results of the study showed that the control group was much more divided in neural activation rates between past substance abusers and non–substance abusers than the schizophrenia group. Whereas the memory-processing brain regions of the formerly substance abusing participants in the control group were far more active during memory tests than the non–substance abusing controls, there was little to no difference in neural activity between the formerly substance abusing schizophrenic participants and non–substance abusing schizophrenic participants. Schizophrenia patients were much less accurate than the controls on all tasks, but these findings indicate that substance abuse may have a relatively smaller impact on the base-level working memory of schizophrenics compared to those without.
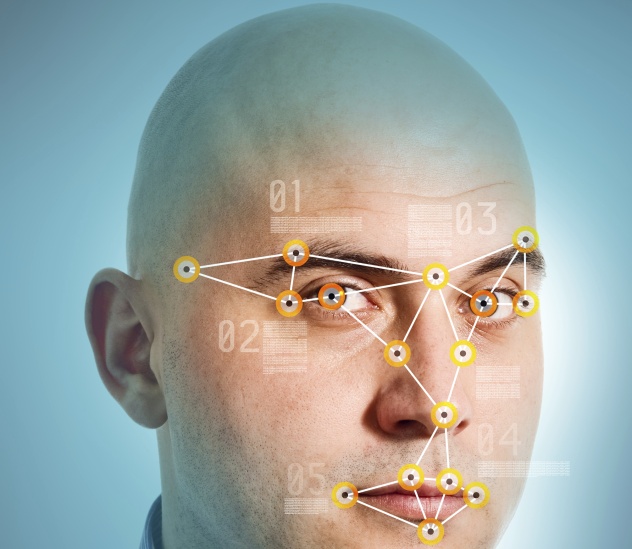
7 Schizophrenics Have Trouble Identifying Facial Expressions But Process Them More
How many times have you awkwardly run into that one person whose name you just can’t ever seem to recall, but you recognize their face every time? It’s moments like those that seriously make you wonder about what your memory will be like a decade from now. In a report on the interaction between cognition and emotions in schizophrenia, Dr. Quintino R. Mano and Dr. Gregory G. Brown cited a number of peculiar findings about the working memory patterns of schizophrenia patients, one of which had to do with simple facial recognition. It was found that while schizophrenia often causes those with the condition to have difficulty expressing and identifying facial emotions, schizophrenia patients also show a significantly heightened rate of automatic and implicit processing of facial emotions.
6 Siblings Of Schizophrenics Have Different Brain Activity Than Others
Dr. Alan Ceaser and associates conducted working memory tests with the participants split into three groups: schizophrenia patients, their siblings without schizophrenia, and a control group of healthy participants without the condition or any direct relationship to people with the condition. The results of the study showed that the patient and sibling group, but not the control group, exhibited different neural reactions to changes in dopamine availability than healthy controls. This supports the hypothesis of excess dopamine being a key player in the emergence of schizophrenic symptoms. The most important implication of the study is that there are abnormal neural activity spikes in the dorsolateral prefrontal cortex (DLPFC), cerebellum, and striatum in both schizophrenia patients and those at risk for schizophrenia—this includes the brothers and sisters of those with the condition.
5 Male Schizophrenic Smokers Are More Susceptible To Nicotine Withdrawal
The subtle neurocognitive deficits of schizophrenia patients can even be observed in the brain’s reaction to nicotine withdrawal. The Clinical Psychiatry Research Center at Tabriz University of Medical Sciences conducted a study to examine the effect of short-term nicotine abstinence on schizophrenic smokers. The 45 participants, all male schizophrenic smokers, were split into three groups: one group that would abstain from smoking for one night, a second group that would use a nicotine patch after avoiding smoking for a night, and a third control group with no intervention at all. Each participant was given a visuospatial memory test at the beginning of the experiment and the following morning, after the intervention. The nicotine patch group and the freely smoking group showed no significant difference in scores between either test, but the group that was withheld from both smoking and nicotine patch use exhibited significantly worse test scores after the intervention. The study concluded that nicotine abstinence causes visuospatial deficits in male smokers with schizophrenia.
4 Gender Affects Schizophrenia Symptoms
Few people really take into account the subtle differences that gender can make on the manifestation of a psychological disorder, let alone schizophrenia, but the effects are very real. It’s understood by many in the field of psychology that schizophrenia often, if not always, accompanies visual perceptual organization impairment—particularly in those patients with rough social histories. Until recently, there was not a complete understanding of just how intensely gender differences can affect the visuospatial deficits in question. Dr. Jamie Joseph and associates at Rutgers University conducted a study to investigate the relationship between disorganized schizophrenic symptoms and gender. The tools used to measure the relationship were specially designed perceptual organization tasks: the Countour Integration Task and the Ebbinghaus Illusion. The participant sample consisted of 43 females and 66 males. The results showed that while females (with more relatively intact bottom-up grouping skills) performed more impressively on the Contour Integration Task, males (with more top-down-oriented grouping skills) performed better on the Ebbinghaus Illusion task. This supports the notion that sex differences are an important factor to consider when weighing in on the visual-perceptual impairments caused by schizophrenia.
3 Younger Schizophrenics Aren’t Being Treated As Effectively
Psychological treatment has come a long way since the mid-19th century. These days, we tend to lean more toward the clinical communication and behavior-analysis method of approach than the “let’s try poking your crazy out with a literal icepick” approach. Despite the advancements in technology and basic human decency, there is some evidence to show that the relationship between age and quality of psychological care doesn’t necessarily improve in a linear fashion as one gets older. In 2013, the Canadian Journal of Psychiatry published findings that show the results of medical-administrative data analyses run over adult schizophrenia patients in Quebec for two years. The results showed that 77 percent of patients aged 30 and over were receiving adequate pharmacological treatment, compared to only 47 percent of patients aged 18–29. The fact that schizophrenia has been documented to be better-treated in the earlier phases of the disease makes this a concerning discovery.
2 Schizophrenics Have Lower Sex Drive
Scientists at the Clinic for Young Schizophrenics ran a study in 2014 measuring the psychosexual tendencies of 45 young adults with schizophrenia. The 45 young adults were compared to 61 young adults without the disease as a control group. The results found that a smaller number of the schizophrenia patients had a sexual partner or had ever had sexual intercourse compared to the control group. More men with schizophrenia who were being treated with risperidone or olanzapine reported issues with arousal than men in the control group. Proportionally, the schizophrenia patient group demonstrated an increased chance of developing negative psychosexual tendencies compared to the control group. This doesn’t mean that anyone should start substituting the word “schizophrenic” for prude—schizophrenia doesn’t erase sexual urges or instantly overstimulate them. These findings only serve to play down the misconception that mental pathology instantly implies hypersexuality.
1 Schizophrenia Is Related To Low Appetite Control
At the Department of Psychiatry at the University of Montreal, a study was conducted in 2012 in order to examine appetite regulation and metabolic differences between schizophrenia patients and a healthy control group. Even if you don’t have a doctorate hanging on your wall, chances are that you’re somewhat familiar with the horror stories that center on metabolism dysfunctions caused by psychiatric treatment gone wrong; the study took this into account as well, measuring the relationship between food cravings and antipsychotic medication dosages. The results showed that only schizophrenic patients demonstrated specific cerebral responses in the parahippocamus, thalamus, and middle frontal gyri to appetite stimulation. Schizophrenic patients’ parahippocampal activity and related hunger levels both increased linearly over time. It was found that medication dosage had a strong positive correlation with food cravings, and also that the severity of the disease was negatively correlated with dietary restraint. The findings show that not only does schizophrenia lend itself to a weakened ability to control the appetite, but also that the antipsychotic drugs used to treat the disease may also drastically exacerbate the dietary symptoms. I was raised on the nation’s capital’s concrete, spent three years eating swordfish and terrible barbeque in the Massachusetts mountains, took a nap, and woke up in this weird dimension they call Long Island to get a doctorate in psychology. I can give you a rough play-by-play on what’s happening in a Spanish soap opera and teach you a lot of Chinese curse words. Slam poetry, rock climbing, marathon running, Muay Thai, Buddhism, electronic music, and stupid YouTube videos keep me sane—if you like any of those, you go on the pretty cool person list. You can also check out my website, Instagram, or Twitter.